C-terminal modification of the insulin B:11-23 peptide creates superagonists in mouse and human type 1 diabetes.
Wang, Y., Sosinowski, T., Novikov, A., Crawford, F., Neau, D.B., Yang, J., Kwok, W.W., Marrack, P., Kappler, J.W., Dai, S.(2018) Proc Natl Acad Sci U S A 115: 162-167
- PubMed: 29255035
- DOI: https://doi.org/10.1073/pnas.1716527115
- Primary Citation of Related Structures:
5UJT, 6BLQ, 6BLR, 6BLX - PubMed Abstract:
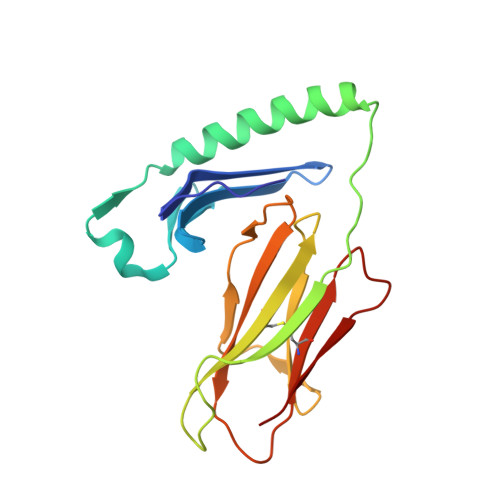
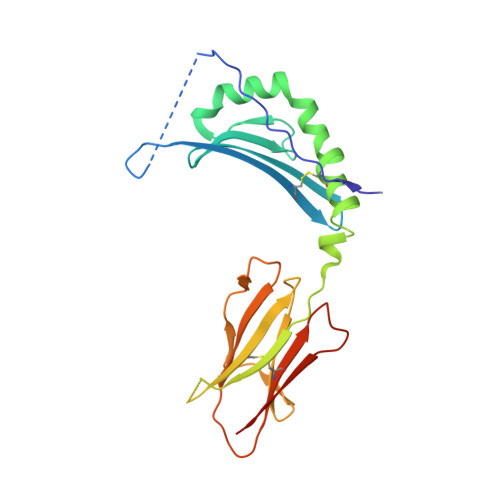
A polymorphism at ¦Â57 in some major histocompatibility complex class II (MHCII) alleles of rodents and humans is associated with a high risk for developing type 1 diabetes (T1D). However, a highly diabetogenic insulin B chain epitope within the B:9-23 peptide is presented poorly by these alleles to a variety of mouse and human CD4 T cells isolated from either nonobese diabetic (NOD) mice or humans with T1D. We have shown for both species that mutations at the C-terminal end of this epitope dramatically improve presentation to these T cells. Here we present the crystal structures of these mutated peptides bound to mouse IA g7 and human HLA-DQ8 that show how the mutations function to improve T-cell activation. In both peptide binding grooves, the mutation of B:22R to E in the peptide changes a highly unfavorable side chain for the p9 pocket to an optimal one that is dependent on the ¦Â57 polymorphism, accounting for why these peptides bind much better to these MHCIIs. Furthermore, a second mutation of the adjacent B:21 (E to G) removes a side chain from the surface of the complex that is highly unfavorable for a subset of NOD mouse CD4 cells, thereby greatly enhancing their response to the complex. These results point out the similarities between the mouse and human responses to this B chain epitope in T1D and suggest there may be common posttranslational modifications at the C terminus of the peptide in vivo to create the pathogenic epitopes in both species.
Organizational Affiliation:
Department of Biomedical Research, National Jewish Health, Denver, CO 80206.