Recurrent XPO1 mutations alter pathogenesis of chronic lymphocytic leukemia.
Walker, J.S., Hing, Z.A., Harrington, B., Baumhardt, J., Ozer, H.G., Lehman, A., Giacopelli, B., Beaver, L., Williams, K., Skinner, J.N., Cempre, C.B., Sun, Q., Shacham, S., Stromberg, B.R., Summers, M.K., Abruzzo, L.V., Rassenti, L., Kipps, T.J., Parikh, S., Kay, N.E., Rogers, K.A., Woyach, J.A., Coppola, V., Chook, Y.M., Oakes, C., Byrd, J.C., Lapalombella, R.(2021) J Hematol Oncol 14: 17-17
- PubMed: 33451349
- DOI: https://doi.org/10.1186/s13045-021-01032-2
- Primary Citation of Related Structures:
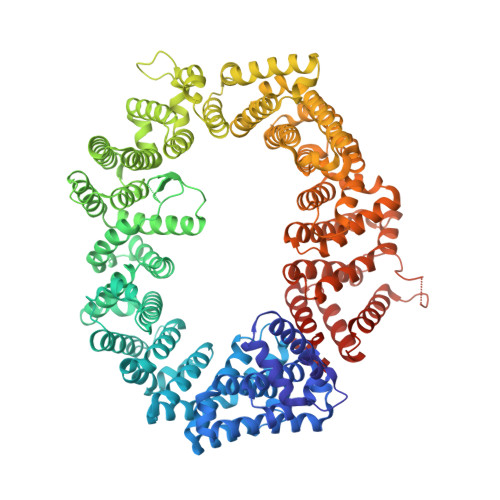
6XJP, 6XJR, 6XJS, 6XJT, 6XJU, 7L5E - PubMed Abstract:
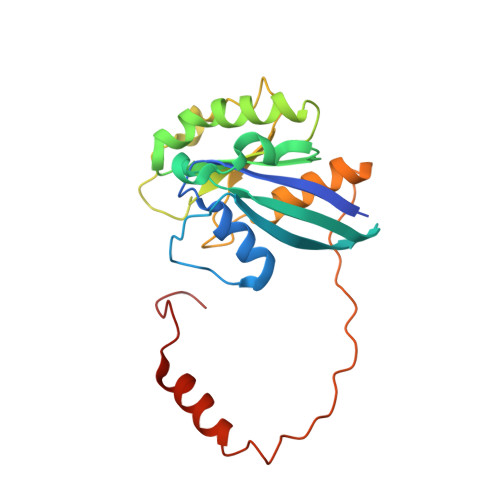
Exportin 1 (XPO1/CRM1) is a key mediator of nuclear export with relevance to multiple cancers, including chronic lymphocytic leukemia (CLL). Whole exome sequencing has identified hot-spot somatic XPO1 point mutations which we found to disrupt highly conserved biophysical interactions in the NES-binding groove, conferring novel cargo-binding abilities and forcing cellular mis-localization of critical regulators. However, the pathogenic role played by change-in-function XPO1 mutations in CLL is not fully understood. We performed a large, multi-center retrospective analysis of CLL cases (N?=?1286) to correlate nonsynonymous mutations in XPO1 (predominantly E571K or E571G; n?=?72) with genetic and epigenetic features contributing to the overall outcomes in these patients. We then established a mouse model with over-expression of wildtype (wt) or mutant (E571K or E571G) XPO1 restricted to the B cell compartment (E?-XPO1). E?-XPO1 mice were then crossed with the E?-TCL1 CLL mouse model. Lastly, we determined crystal structures of XPO1 (wt or E571K) bound to several selective inhibitors of nuclear export (SINE) molecules (KPT-185, KPT-330/Selinexor, and KPT-8602/Eltanexor). We report that nonsynonymous mutations in XPO1 associate with high risk genetic and epigenetic features and accelerated CLL progression. Using the newly-generated E?-XPO1 mouse model, we found that constitutive B-cell over-expression of wt or mutant XPO1 could affect development of a CLL-like disease in aged mice. Furthermore, concurrent B-cell expression of XPO1 with E571K or E571G mutations and TCL1 accelerated the rate of leukemogenesis relative to that of E?-TCL1 mice. Lastly, crystal structures of E571 or E571K-XPO1 bound to SINEs, including Selinexor, are highly similar, suggesting that the activity of this class of compounds will not be affected by XPO1 mutations at E571 in patients with CLL. These findings indicate that mutations in XPO1 at E571 can drive leukemogenesis by priming the pre-neoplastic lymphocytes for acquisition of additional genetic and epigenetic abnormalities that collectively result in neoplastic transformation.
Organizational Affiliation:
Division of Hematology, Department of Internal Medicine, The Ohio State University, 460 OSUCCC, 410 West 12th Avenue, Columbus, OH, 43210, USA.